New Patients
Existing Patients
New Patients
Existing Patients
New Patients
Existing Patients
New Patients
Existing Patients
If your dentist says a tooth needs a root canal, don’t panic — this treatment is a well-established, predictable way to stop pain and save a natural tooth. Modern root canal therapy uses precise instruments and effective pain control so most patients experience far less discomfort than they expect. In many cases, treatment prevents the need for extraction and preserves your long-term dental health.
At RGV Smiles by Dr. Rocky L. Salinas, DDS, PA, we focus on delivering careful, evidence-based care while keeping patient comfort front and center. Our team combines up-to-date techniques with a gentle approach so you can move through treatment with confidence and a clear understanding of your options.
Maintaining your natural tooth whenever feasible is one of dentistry’s guiding principles. A root canal removes diseased tissue from inside the tooth while leaving the external structure intact, allowing you to keep the tooth in function for years — often for life. Preserving the tooth also helps maintain the proper alignment of neighboring teeth and supports healthy jawbone over time.
Contemporary root canal procedures are designed to be efficient and minimally invasive. Advances in instrumentation, irrigation, and filling materials have improved the predictability of outcomes and reduced recovery time. When paired with an appropriate restoration, such as a crown, a treated tooth will frequently withstand normal chewing forces without further complications.
Choosing to preserve a tooth through endodontic therapy avoids many of the long-term consequences of extraction, such as shifting teeth, bite changes, and the eventual need for replacement options like bridges or implants. In short, root canal therapy is often the conservative solution that supports both oral health and day-to-day function.

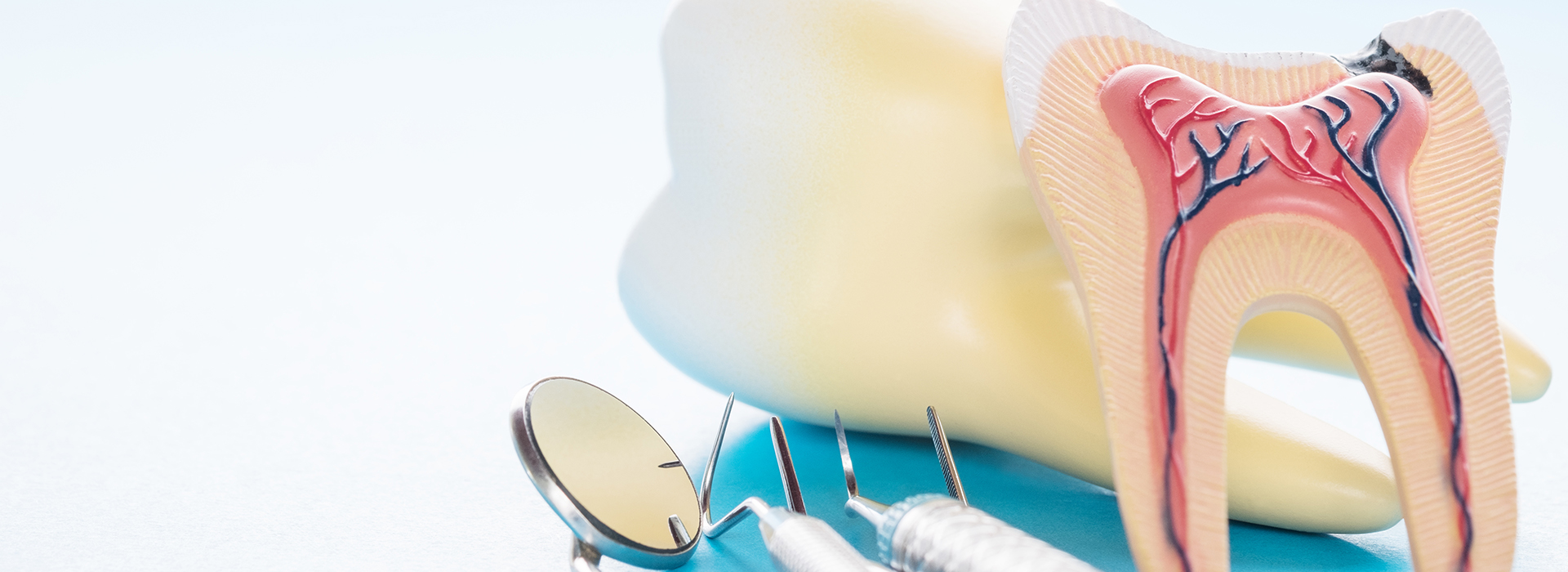
Inside every tooth is a small chamber containing nerves, blood vessels, and connective tissue — the dental pulp. This tissue plays an important role while a tooth is developing, but once the tooth is fully formed it no longer needs the pulp to survive. When bacteria invade the inner chamber through deep decay, cracks, or trauma, the pulp can become inflamed or die, which often leads to infection and discomfort.
Symptoms that commonly signal pulpal involvement include persistent or worsening tooth pain, heightened sensitivity to hot and cold that lingers after the stimulus is removed, and pain when biting or tapping the tooth. In some cases a tooth may darken in color or cause localized gum swelling. Not every problem is obvious, however — some infected teeth show little pain but reveal issues on X-rays during routine exams.
Early diagnosis matters because a tooth treated before a widespread infection develops usually has a simpler procedure and smoother recovery. When the pulp is compromised but the tooth still has adequate structure and bone support, root canal therapy can remove the source of infection while preserving function and appearance.
Many of the situations below commonly lead to root canal therapy. If you notice any of these signs, prompt evaluation is advised.
Pain that lingers or intensifies — especially pain that wakes you at night — often points to deep decay or an infection that has reached the inner tissues of the tooth. This is one of the most common reasons a clinician recommends root canal treatment.
A brief twinge with temperature changes is normal for many people, but prolonged sensitivity that remains after drinking hot or cold beverages can indicate an inflamed or dying nerve inside the tooth.
Discomfort during chewing or when pressure is applied often suggests the inner tissues are irritated or infected. This symptom is especially notable when the tooth feels different from others in the same area.
A tooth that has darkened in color following trauma may have injured or necrotic pulp tissue. Discoloration alone doesn’t always mean a root canal is needed, but it is a sign that warrants professional assessment.
Structural damage that reaches the deeper parts of the tooth can allow bacteria to enter the pulp chamber. In many cases, treatment to remove the infected tissue is required to prevent further spread and preserve the tooth.
Swollen tissue or an area that occasionally drains fluid can signal an abscess — a collection of infection at the root tip. This condition typically needs root canal therapy to resolve the underlying cause.
Advanced infection can affect the bone that supports a tooth, causing mobility. Treating the infection early gives the best chance for stabilizing the tooth and restoring health to surrounding tissues.

Prompt attention when a tooth is behaving abnormally improves the likelihood of straightforward treatment and reduces the risk of complications. As an infection progresses, it can spread beyond the root tip, damage surrounding bone, and require more extensive care. Early intervention generally simplifies the procedure and shortens recovery.
Not every tooth that hurts will require a root canal, and a comprehensive exam — including X-rays when appropriate — helps determine the true cause. Sometimes a less invasive solution will resolve the problem; other times endodontic treatment is the most reliable pathway to removing infection and preserving function.
Delaying care can lead to worsening pain, swelling, or the need for emergency treatment. For teeth that show radiographic signs of root-end involvement or structural breakdown, timely therapy supports better healing and reduces the chance of losing the tooth altogether.
Root canal therapy is performed with local anesthesia to keep you comfortable, and in many practices additional comfort measures are available for anxious patients. The dentist creates a small opening in the tooth to reach and remove the infected pulp, then carefully cleans and shapes the canals to prepare them for filling.
The number of appointments varies by case. Some teeth can be treated in a single visit; others need two or more visits when infection control, anatomy, or restorative planning makes that preferable. Treatment time depends on factors such as how many canals the tooth has and whether an active infection needs to be managed first.
Once the canals are cleaned and disinfected, they are sealed with a biocompatible material to prevent recontamination. Afterward, the tooth is restored with a permanent filling or crown to rebuild strength and function. Your clinician will explain restorative timing and any temporary measures used between appointments.

After treatment, it’s normal to experience mild tenderness or sensitivity for a few days as surrounding tissues recover. Over-the-counter pain relievers typically manage these symptoms effectively; your dentist will advise you if additional medication is necessary. Maintaining good oral hygiene and following post-procedure guidance helps support healing.
A treated tooth is often restored with a crown or another durable restoration to protect it from fracture and restore full chewing function. Until the permanent restoration is placed, try to avoid chewing hard or sticky foods on the treated side. Keeping the restoration timeline helps ensure the long-term success of the procedure.
Regular dental checkups allow your care team to monitor the treated tooth and surrounding structures. With proper restoration and routine care, teeth that have undergone root canal therapy can remain functional for many years. If you notice new or worsening pain, swelling, or drainage after treatment, contact your dental office for evaluation.
At RGV Smiles by Dr. Rocky L. Salinas, DDS, PA, our objective is to help you make informed decisions and to carry out treatment with precision and compassion. We take time to explain the process, answer questions, and provide care options tailored to your needs.
Summary — Root canal therapy is a reliable, tooth-preserving treatment for infections and deep damage to the inner tooth. When detected early and followed by appropriate restoration, it relieves pain, resolves infection, and restores function. If you have concerns about persistent tooth pain, sensitivity, or a damaged tooth, please contact us for more information and to schedule an assessment.

Root canal therapy is a treatment that removes infected or inflamed pulp from inside a tooth to stop infection and preserve the remaining tooth structure. The procedure cleans and shapes the internal canals, disinfects the space, and seals it with a biocompatible filling to prevent recontamination. When followed by an appropriate restoration, such as a permanent filling or crown, the treated tooth can often continue to function for many years.
Preserving a natural tooth through endodontic therapy helps maintain proper chewing function and prevents adjacent teeth from shifting into the vacant space. Modern instruments, improved irrigants, and more predictable filling materials have increased the success and comfort of the procedure. In many cases, a root canal avoids the need for extraction and more extensive restorative work later on.
Common signs that a tooth may require root canal treatment include persistent or severe toothache, heightened sensitivity to hot or cold that lingers, and pain when biting or tapping the tooth. Other indicators include localized gum swelling, a recurring drainage or pimple on the gum, and discoloration of the tooth following trauma. Not every symptomatic tooth needs a root canal, but these symptoms warrant prompt evaluation to determine the cause.
Some infected teeth cause minimal or no pain yet show changes on X‑rays during routine exams, which is why regular dental checkups are important. Early detection usually allows for a simpler procedure and smoother recovery. If you notice new symptoms or a tooth that feels different, scheduling an exam sooner improves treatment options.
A dentist begins with a thorough clinical exam that includes a review of symptoms, visual inspection, and tests for percussion and bite sensitivity to identify a problematic tooth. Radiographs (X‑rays) are commonly used to assess the extent of decay, detect periapical changes at the root tip, and evaluate the surrounding bone. When indicated, additional tests such as pulp vitality testing help determine whether the pulp is inflamed, infected, or no longer viable.
Diagnosis considers the tooth's restorability, the presence of fractures, and the patient’s overall oral health to recommend the most conservative, effective option. In some situations referral to an endodontist is advised for complex anatomy or difficult access. A clear explanation of findings and treatment choices helps patients make informed decisions about care.
The procedure starts with local anesthesia to numb the tooth and surrounding tissues so patients remain comfortable throughout treatment. The dentist creates a small access opening, removes infected or inflamed pulp, and carefully cleans and shapes the canal system using specialized instruments and irrigating solutions. After disinfection, the canals are sealed with a biocompatible filling material to prevent bacteria from reentering.
Some teeth can be treated in a single visit while others require two or more appointments depending on infection severity, anatomy, or restorative planning. If a temporary filling is placed between visits, your clinician will explain timing and next steps for the permanent restoration. The final restoration, often a crown, restores strength and function to the treated tooth.
During the procedure most patients feel little to no pain because local anesthesia effectively numbs the area and modern techniques prioritize comfort. For patients with high anxiety, additional comfort measures such as nitrous oxide or other sedation options may be available and can be discussed with your dentist. Clear communication about sensations and the treatment plan helps reduce stress and ensures a smoother experience.
After treatment it is normal to experience mild tenderness or sensitivity for a few days as surrounding tissues heal, and over‑the‑counter pain relievers typically manage these symptoms. If symptoms persist or worsen, you should contact your dental provider for reassessment because prolonged or increasing pain may indicate a complication. Following post‑op instructions and avoiding hard or sticky foods on the treated side until the final restoration is placed helps protect the tooth during recovery.
Immediately after treatment avoid chewing on the treated tooth until a permanent restoration is placed to reduce the risk of fracture. Maintain excellent oral hygiene by brushing twice daily and flossing carefully around the treated area, and follow any specific rinsing or medication instructions provided by your dentist. Keeping scheduled follow‑up appointments ensures your clinician can monitor healing and complete the necessary restoration.
Long‑term success depends on protecting the tooth with an appropriate crown or filling and addressing any underlying issues such as deep decay or cracks that contributed to the problem. Report new or worsening symptoms like swelling, recurrent drainage, or increasing pain so the tooth can be rechecked promptly. Routine dental visits and preventive care reduce the chance of future complications.
Teeth that receive thorough endodontic treatment and timely restorative protection can last many years and often remain functional for a lifetime. Success depends on factors such as the quality of the root canal filling, the type of restoration placed, the amount of remaining tooth structure, and the patient’s oral hygiene. Teeth that are weakened by extensive decay or fractures may have a higher risk of future problems if not adequately restored.
Regular dental checkups and proper home care help identify any changes early so they can be addressed before they threaten the tooth. If a treated tooth develops recurrent infection or structural failure, retreatment or referral to a specialist may be recommended. With attentive care, preserved natural teeth typically provide better long‑term outcomes than extracted teeth replaced by removable appliances alone.
The primary alternative to root canal therapy is extraction of the affected tooth, after which tooth replacement options such as dental implants, bridges, or removable prostheses can be considered. Each replacement choice has different implications for adjacent teeth, bone preservation, and function, so the decision should weigh clinical factors and long‑term oral health goals. In some cases less invasive treatments or monitoring may be appropriate if the pulp problem is reversible or early.
Preserving the natural tooth is generally preferred when feasible because it maintains normal chewing function and helps protect neighboring teeth and bone. Your dentist can explain the risks and benefits of extraction and replacement versus endodontic treatment to help you choose the most conservative, effective approach. Timely evaluation and a clear restorative plan improve the likelihood of a favorable outcome regardless of the chosen path.
You should seek prompt dental attention for a tooth problem if you experience severe or worsening pain, significant swelling of the face or gums, fever, or persistent drainage from the gum near a tooth. These signs can indicate a spreading infection that may require urgent intervention to control pain and prevent complications. Delaying care increases the risk that the infection will affect surrounding bone or other tissues and may necessitate more extensive treatment.
If the situation feels like an emergency or is accompanied by difficulty breathing or swallowing, seek immediate medical care or emergency services. For less severe but concerning symptoms, contact your dental office to arrange an evaluation so appropriate treatment can begin. Early diagnosis and treatment usually lead to simpler procedures and better healing.
At RGV Smiles by Dr. Rocky L. Salinas, DDS, PA our approach to root canal therapy emphasizes patient comfort, clear communication, and evidence‑based techniques. We use effective local anesthesia and modern instruments to reduce procedural time and improve predictability, and we explain each step so patients understand what to expect. When appropriate, additional comfort options and careful scheduling are offered to accommodate anxious or complex cases.
After treatment our team provides individualized post‑op instructions and coordinates timely restorative care to protect the treated tooth and support long‑term success. Routine follow‑up appointments allow us to monitor healing and address any concerns quickly. Our goal is to combine clinical expertise with compassionate care so patients feel confident throughout diagnosis, treatment, and recovery.

Ready to take the next step toward a healthier, brighter smile?
Contacting RGV Smiles by Dr. Rocky L. Salinas, DDS, PA is the first step! Our supportive team is available to assist with all your needs, from booking routine care to discussing advanced cosmetic services. Simply call or use our online form to connect with us today. We make it easy to prioritize your oral health!